Sep 15, 2022
More Than Half of US Hospitals Expect to Lose Money This Year
, Bloomberg News
(Bloomberg) -- An eight-hour emergency room wait. The closing of a local clinic in a high-poverty area of rural Arkansas. Dwindling maternity wards.
These are some of the outcomes of the financial pain US hospitals are feeling as spiking costs dictate sometimes-dire decisions. And it’s not getting any better, according to a report Thursday.
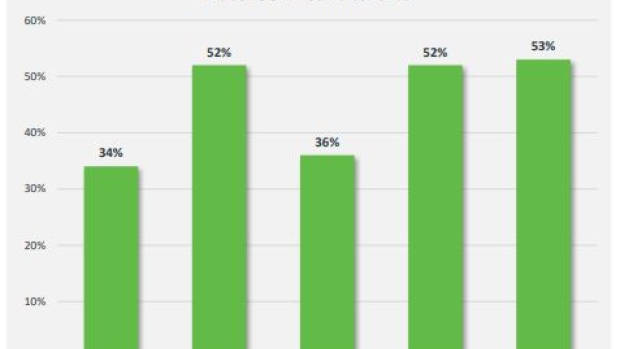
More than half -- 53% -- of US hospitals expect to lose money this year, according to the report prepared by consulting firm Kaufman Hall for the American Hospital Association. Facilities are scrambling not only to fill jobs but to cope with sharply higher costs for labor and supplies, all while treating Covid-19 and other patients, many of whom arrive sicker because they have put off treatment.
Operating margins will fall 37% this year in an optimistic scenario -- and 133% in the worst case, compared with pre-pandemic, according to the report. A large part of the spike in costs came from having to pay travel nurses during pandemic surges and spiking turnover. That need has waned at many facilities.
But labor costs remain higher than before the pandemic as hospitals compete with employers -- like fast-food restaurants -- that used to pay less. Kaufman Hall forecasts expenses for US hospitals this year will climb $135 billion over last year’s already-elevated levels. Labor will make up $86 billion of that.
Main Line Health, a not-for-profit system with five hospitals and other facilities around Philadelphia, lost $102 million in its 2022 fiscal year and $20 million in July alone, losses its Chief Executive Officer Jack Lynch called “unsustainable.”
The suburban Philadelphia system has seen a surge of maternity and other patients after the recent closures of two local hospitals, Lynch said -- all while struggling to fill more than 1,500 jobs and treating sicker patients.
Most of his chain’s patients have Medicare or Medicaid, and those reimbursements come up far short of what’s needed, said Lynch, who spoke on a call hosted by AHA Thursday, along with two other CEOs.
At Trinity Health, a Catholic non-profit chain of almost 90 hospitals, the rate of patients leaving emergency rooms without being seen has doubled since before the pandemic, said CEO Michael Slubowski, as lengthy treatments for sicker patients stretches waiting time.
The Michigan-based chain has 16% of its registered nursing jobs open. When its Boise hospital had a small Covid-19 surge this summer, a shortage of staff forced it to treat patients in the ER instead of in hospital rooms.
“Most US hospitals are only one Covid-19 or flu surge away from crisis,” Slubowski said.
Cash on hand at Ouachita County Medical Center in rural Arkansas “is lower than I have ever seen” in 35 years, said CEO Peggy Abbott. That dictated the “heart-wrenching” decision to close a rural health clinic 20 miles away that it operated for 25 years.
“It doesn’t take a mathematician to see that we are hurting,” she said. “In fact, we are bleeding red.”
©2022 Bloomberg L.P.


